Acne vulgaris: Origins, symptoms and current treatments
Acne vulgaris, commonly known as acne, is a chronic inflammatory disease of the skin which affects most adolescents and is the cause of over half of all dermatology consultations. This pathology, which is characterized by a hypersecretion of sebum, can be the cause of physical complications and may also lead to psychological distress. In order to propose the appropriate treatment, a good understanding of this disease requires knowledge of the predisposing factors and of the cellular and molecular mechanisms which lead to the onset of symptoms.
Epidemiology
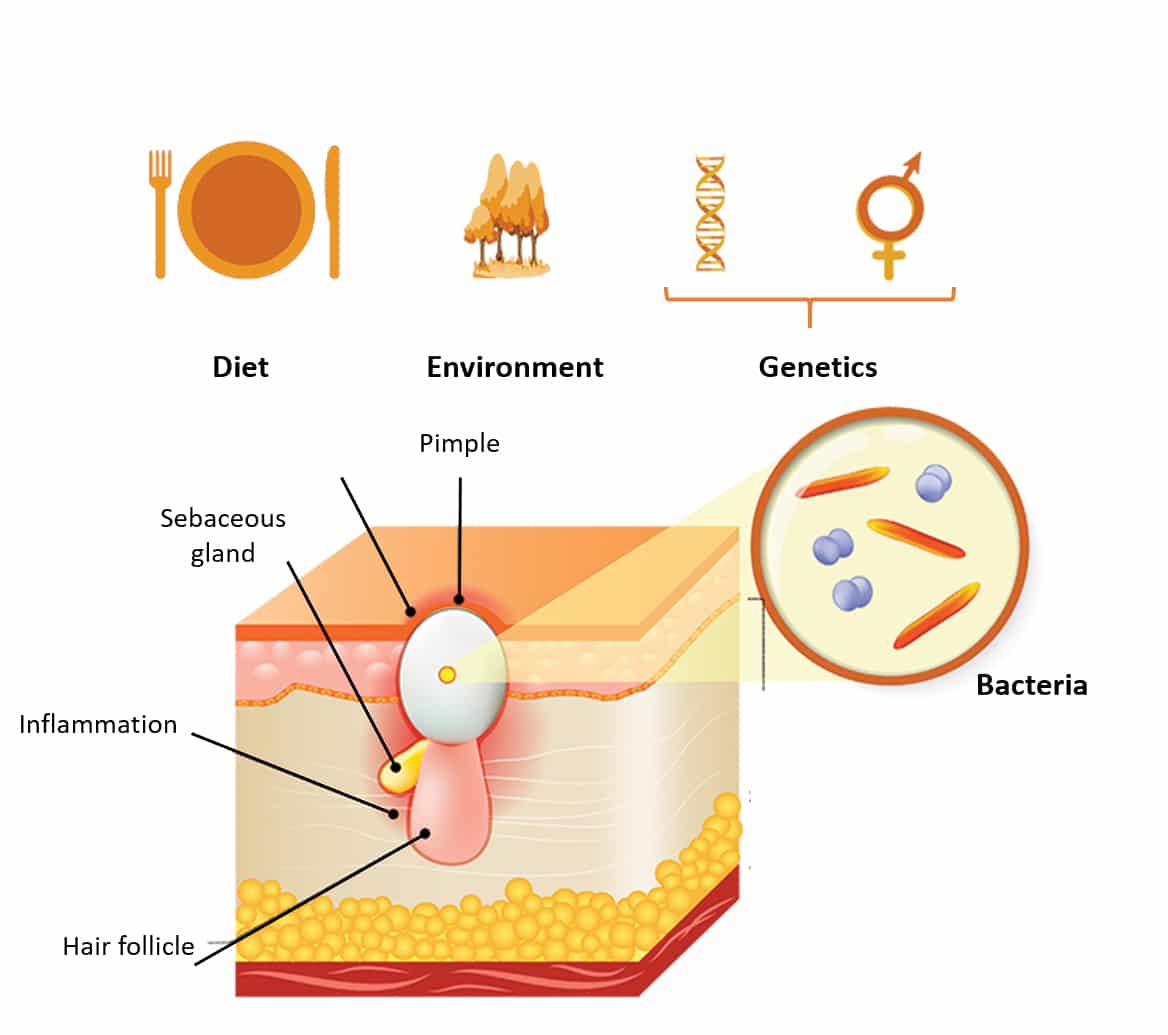
Acne vulgaris is a disease related to hormonal dysfunctions in the pilosebaceous follicle, the end result of which is over-production of sebum by the sebaceous gland. Adolescents are generally the most affected and the findings of epidemiological studies estimate that over 80% of persons suffer from acne during puberty. All ethnic groups are concerned and with the exception of acne during pregnancy, it is rare for acne to continue after reaching adulthood, especially in men. Comedones and pustules are the principal characteristics of this pathology and appear where the density of pores is the highest: i.e. mainly on the face, the back and the chest. Largely of genetic origin, this dysfunction may also be exacerbated by environmental factors such as diet or pollution (Figure 1).
Origins
The genetic and hormonal component
Under normal conditions, sebum is synthesized and secreted by the sebocytes in the sebaceous gland. Its production, delicately coordinated at the genome level, is dependent on stimulation by androgens. This hormonal stimulation induces the transduction of a signal via translocation towards the nucleus of the androgen receptors initially located in the cytoplasm, finally leading to activation of the genes involved in sebum production.
A greater sensitivity to androgenic hormones, due for example to an abnormal quantity of androgen receptors or to an over-production of androgenic hormones, will cause hypersecretion of sebum (hyperseborrhoea), the main cause of acne.
The dietary component
Although it cannot be the cause of acne, it has been shown that diet may be an exacerbating factor. A diet rich in sugars and fats is thought to stimulate the differentiation and the lipogenic activity (sebum production) of the sebaceous gland cells, the sebocytes.
Figure 1: Causes and origins of acne vulgaris
The environmental component
The presence of bacteria such as Propionibacterium acnes in the pilosebaceous structure is acknowledged as being implicated in the development of the disease. Heavy smoking and alcohol consumption also appear to be factors which may increase the acne condition. Among other environmental factors, stress, urban pollution and exposure to the sun (UV radiation inducing sebum peroxidation), are also recognized as being implicated in the exacerbation of acne symptoms.
Symptoms
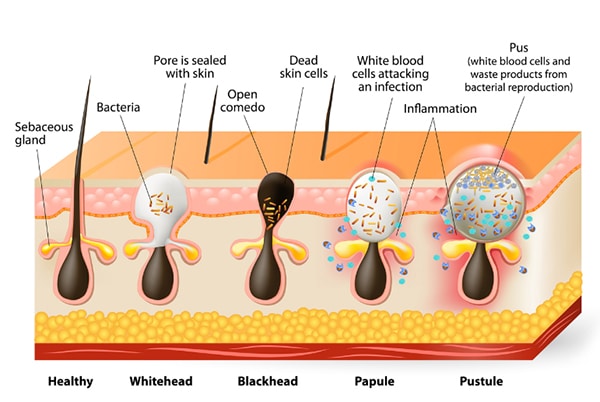
Figure 2: Various forms of acne vulgaris
Symptoms
The clinical diagnosis is performed on the basis of a visual examination of the skin where acne is characterized by lesions due to the obstruction of the hair follicles caused by an over-production of sebum, and also by the dysfunction of the process of keratinocyte differentiation. These lesions may be non-inflammatory (comedones) or inflammatory (pustules, papules, cysts).
The various forms of acne are described on the basis of the severity of the clinical signs (Figure 2):
- Light: less than half of the face is impacted; some open and closed comedones; some papulo-pustules
- Moderate: More than half of the face is impacted; some open or closed comedones; numerous papulo-pustules
- Severe: the whole face is impacted; open or closed comedones; numerous papulo-pustules; rare nodules
- Very severe: highly inflammatory acne with nodules on the whole face
- Cystic: presence of cysts
Complications
Complications may occur in certain cases. The onset of sometimes painful nodules and cysts is one of the very severe forms of acne which will lead to deep scarring and hyperpigmentation. Certain bacteria (Propionibacterium acnes, Staphylococcus aureus, etc.) are well known for their implication in the exacerbation of the disease.
Treatments
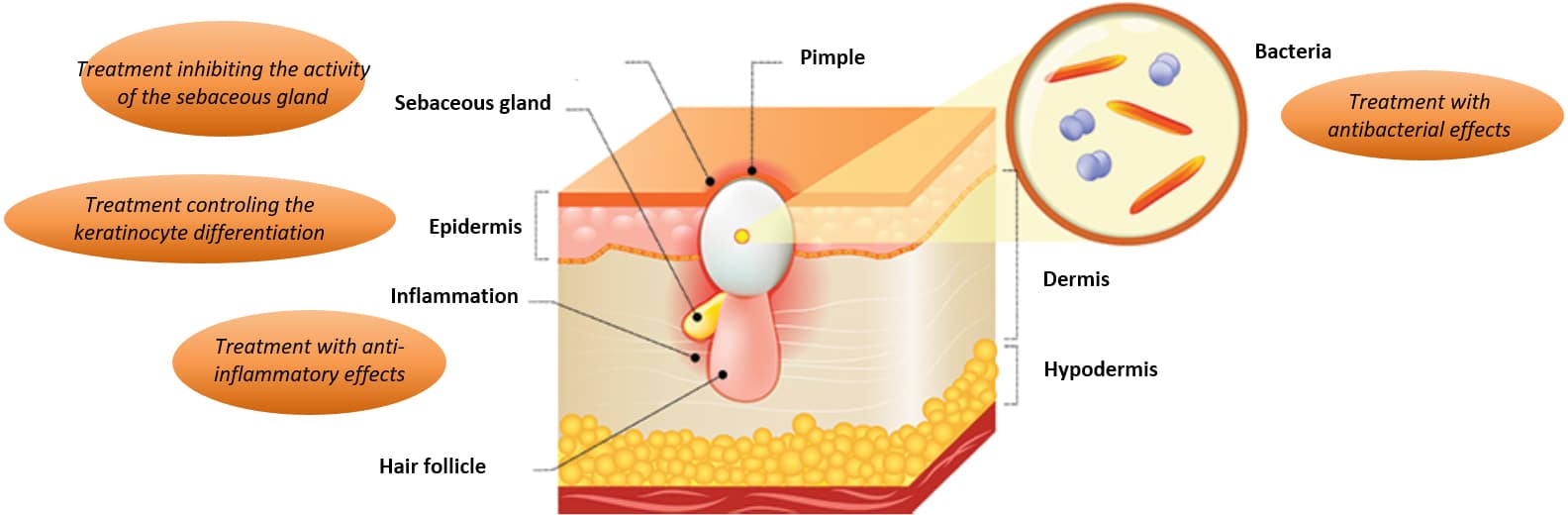
Various types of treatment exist:
- Topical treatments for local application (gel, ointment) in the case of mild acne will act either by controlling the process of keratinocyte differentiation (retinoids), or by bactericidal action (benzoyl peroxide)
- Oral treatments prescribed in the case of moderately severe acne will act at the hormonal level (cyproterone acetate, finasteride, oral contraceptives)
- Oral antibiotic treatments may also be prescribed in the case of severe acne, in combination with a topical treatment
- Isotretinoin is a molecule recommended for severe acne. Although the mechanism of action of this molecule is not completely known, isotretinoin seems to be implicated in the reduction of the development of the sebaceous gland, which could affect sebum production. The molecule is also thought to exhibit anti-inflammatory properties. This treatment, known for its teratogenic effects, is prescribed in women at the same time as oral contraception
Figure 3: Mechanisms of anti-acne treatments
The currently used anti-acne treatments are mainly designed to reduce the onset of the clinical signs (Figure 3). At the present time, there is no treatment which can prevent and effectively treat this pathology.
Related posts
Check out Bioalternatives’ updates and experience new testing ideas
- Bioassays, models and services
- Posts and publications
- Events