Physiology and functions of the sebaceous gland
The human skin has an average of 2,000,000 sebaceous glands, distributed with a density of approximately 400 to 900 glands per cm² on the face. The sebaceous gland is an organ located in the dermis. Its role is to synthesise and secrete sebum which is a component of the hydrolipidic film. The purpose of sebum is to protect the skin from damages caused by external factors and from dehydration. Sebum also maintains the suppleness of skin and hair.
Physiology of the sebaceous gland
The pilosebaceous compartment
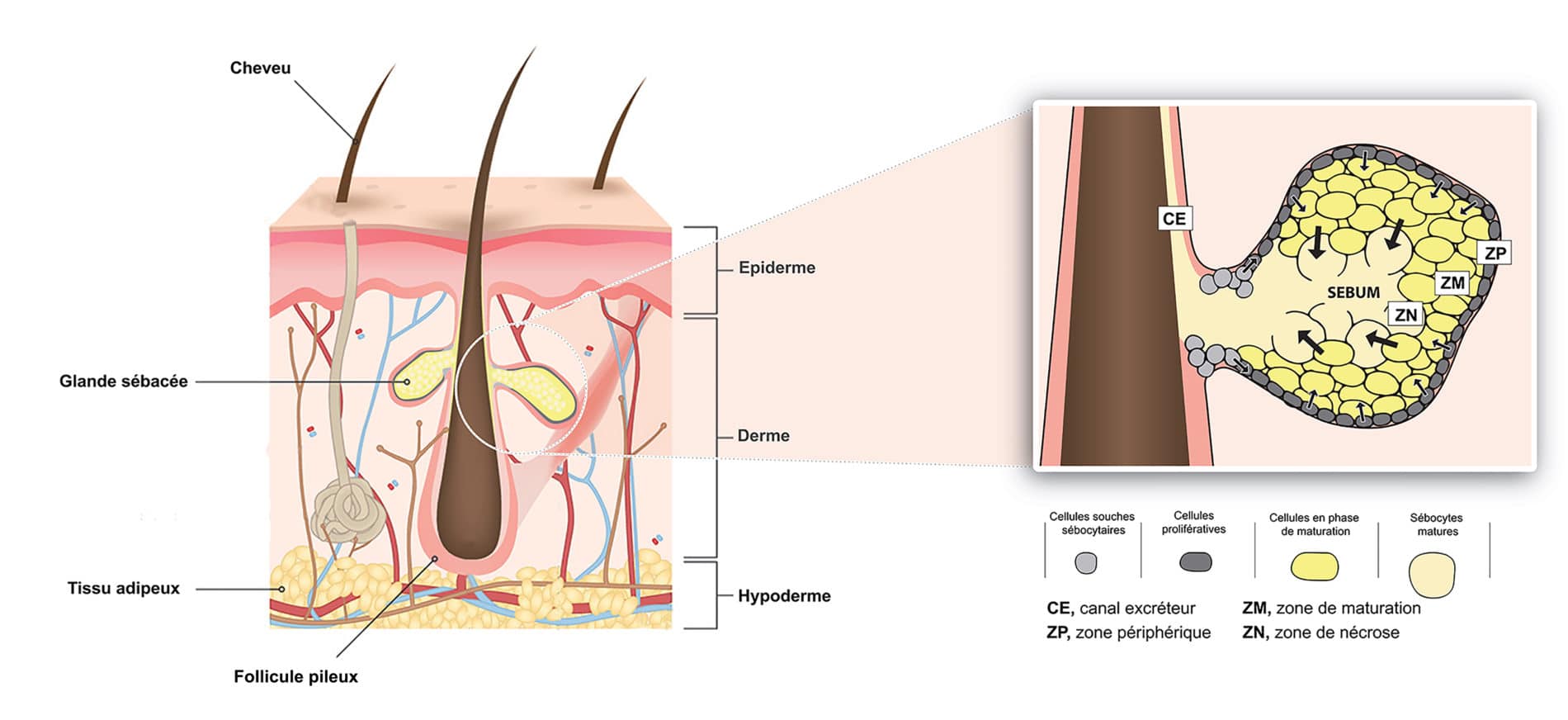
The sebaceous gland is associated with a hair follicle, forming the pilosebaceous unit. Located in the dermis, the sebaceous gland is connected to the hair follicle by the excretory duct. Sebum is secreted along the hair root and up to the skin surface via this canal (Figure 1).
Sebocytes
Sebocytes are the cells which constitute the major part of the sebaceous gland. They are responsible for the synthesis and secretion of sebum.
The sebaceous gland is composed of three types of cells which are distributed in three distinct concentric zones.
- The peripheral zone, or germinative layer: the cells located around the periphery of the sebaceous gland form a monolayer of non-differentiated proliferative cells. They express stem cell markers (KRT15, TNC, KRT75, FST), as well as the early sebocyte marker, keratin 7. They are characterized by a flattened appearance and by the presence of a nucleus. During the differentiation process, these cells start a slow process of apoptosis, become filled with lipids and are pushed towards the centre of the sebaceous gland into the maturation zone.
- The maturation zone: during the maturation process, sebocytes increase in volume and express the specific markers of mature sebocytes such as Fatty Acid Desaturase 2 (FASD2) or epidermal membrane antigen (EMA) [Assays: SEBOAR-0003; SEBOAR-0004; SEBO3D-0003; SEBO3D-0004] and gradually synthesize sebum [Assay: SEBOAR-0007; SEBO3D-0005; SEBO3D-0011; SKIN-0041; SKIN-0048].
- The necrosis zone: once mature, sebocytes release their sebum content by the holocrine process, during which the release of sebum occurs via the rupture of the sebocyte membrane. The released sebum then passes through the excretory duct to be finally released at the skin surface.
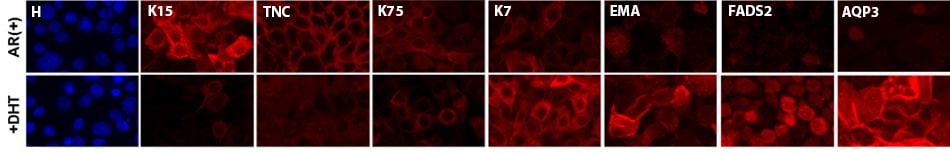
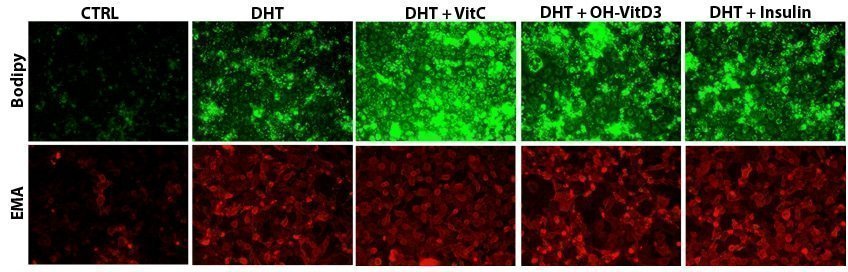
Figure 2: Impact of DHT on differentiation marker expression. Assay performed on a model of human sebocytes expressing androgen receptors
Sebum composition and function
Composition of sebum
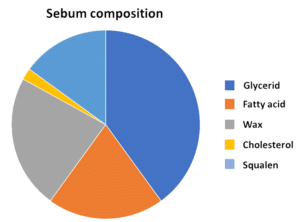
Sebum is a complex lipid mixture composed of:
- Glycerides: 30-50%
- Fatty acids (sapienic acid): 15-30%
- Waxes (wax esters): 26-30%
- Cholesterol: 1.5-2.5%
- Squalene: 12-20%
While most of the lipid components of sebum are also found in other parts of the body, squalene and wax esters remain characteristic components of sebum.
Figure 3: Composition of sebum
The biological functions of sebum
In addition to its role as a protective barrier that reduces skin dehydration, sebum also possesses antibacterial properties, due to the action of oleic and palmitoleic acids, and also anti-oxidant properties, conferred by vitamin E and other substances.
Sebum and skin and hair textures
Inter-individual differences in the level of sebum secretion are responsible for the different types of skin texture: dry skin or brittle hair is the consequence of low sebum secretion, whereas oily skin or greasy hair will be the consequence of a higher sebum secretion, which is known as hyperseborrhoea. This hyper-secretion of sebum may also be the cause of skin changes such as acne.
Regulation of sebum production under normal conditions
Sebum production is a process controlled by various mechanisms.
Hormone regulation
This is the main pathway of regulation of sebum production by sebocytes.
Testosterone is metabolized to dihydrotestosterone (DHT) via 5-alpha reductase [Assay: SEBOAR-0018], testosterone and is the key factor in this regulation pathway. Under the action of DHT, sebocytes activate the signalling pathways involved in lipid synthesis via androgen receptors (AR) that are located in the sebocyte cytoplasm [Assays: SEBOAR-0007 and SEBOAR-0008].
The regulation of sebum production by growth hormones, such as insulin, IGF (Insulin Growth Factor) or hydrocortisone [Assay: SEBOAR-0020] are other pathways of hormone stimulation by acting on the growth of the sebocytes.
Figure 4: Impact of DHT and other lipogenic factors on lipid production (bodipy) and differentiation (EMA).
Assay performed on a model of human sebocytes expressing androgen receptors
Other regulatory factors
Besides the effects of androgen hormones, there are other factors which regulate lipid synthesis.
- Endogenous factors: the lipogenic activity may be influenced by other non-hormonal endogenous lipogenic factors, such as the products of fatty acid metabolism, such as cholesterol or cholecalciferol (vitamin D), or by some molecules of the retinoid family and of its derivatives such as retinoic acid, retinol or vitamin A [Assay: SEBOAR-0019].
- Environmental / exogenous factors: they are implicated in the quality and quantity of secreted sebum.
- Pollution: whether natural or due to human activity (ozone, industry, farming, smoking, etc.), it affects the composition of sebum and is also thought to stimulate its secretion
- Exposure to UV: skin damage caused by the sun’s UV radiation is also a factor with an impact on the quality of the sebum present on the skin surface
- Diet: the presence in diet of certain nutrients, such as certain types of fatty acids (e.g. cholesterol) is also thought to have an impact on the regulation and the quality of the secreted sebum [Assay: SEBOAR-0009]
Related posts
Check out Bioalternatives’ updates and experience new testing ideas
- Bioassays, models and services
- Posts and publications
- Events